At The Barefoot Osteo Warrnambool, we understand that sciatica is a condition that affects millions of people worldwide, often manifesting as sharp, shooting pain that radiates from the lower back down the legs. Osteopathy for sciatica offers a holistic approach to addressing this discomfort by focusing on the root causes and promoting long-term wellness.
Sciatica is caused by irritation or compression of the sciatic nerve—the largest nerve in the body—and can significantly impact daily life. Simple tasks like sitting, walking, or standing can become uncomfortable, and the condition often leads to emotional distress and decreased productivity.
For many, traditional treatments provide only temporary relief, failing to address the underlying issues causing their discomfort. Over time, this can result in chronic pain and frustration. This is where osteopathy for sciatica becomes a transformative option, providing non-invasive care tailored to each individual’s needs. By restoring balance within the musculoskeletal system, reducing nerve compression, and improving alignment, osteopaths help patients regain control and move freely.
Understanding the Sciatic Nerve
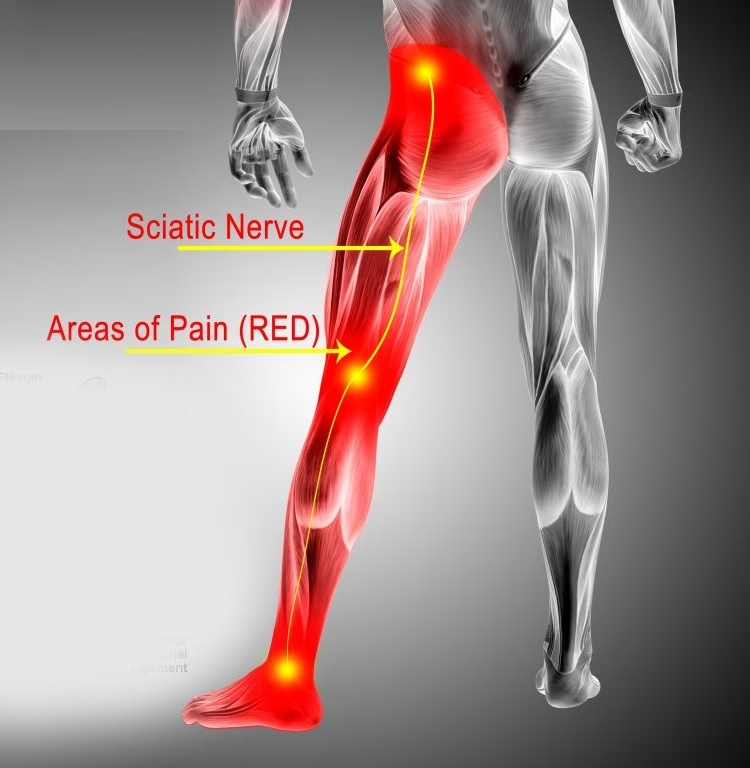
The sciatic nerve plays a crucial role in connecting the lower back, hips, and legs, making it integral to mobility and sensation in the lower body. As the largest nerve in the body, it originates from the lumbar spine, travels through the pelvis, and runs down each leg to the feet. When this nerve becomes irritated or compressed, it can result in the painful symptoms of sciatica.
Common Causes of Sciatica
- Herniated Discs: Displaced spinal discs can press on the sciatic nerve, causing inflammation and pain.
- Piriformis Syndrome: Tightness or spasms in the piriformis muscle—located deep in the buttock—can irritate the sciatic nerve.
- Spinal Stenosis: A narrowing of the spinal canal can compress the nerves, including the sciatic nerve.
- Muscle Imbalances: Poor posture or uneven muscle strength can lead to nerve compression or irritation.
Common Symptoms of Sciatica
Sciatica manifests in a variety of ways, often disrupting everyday activities and diminishing quality of life. Recognizing these symptoms early is key to seeking effective treatment and relief.
- Radiating Pain: Sharp, shooting pain typically starts in the lower back and travels down the leg, sometimes reaching the foot. This pain can vary in intensity, from mild discomfort to debilitating, throbbing sensations that interfere with daily activities.
- Tingling or Numbness: A sensation of pins and needles or loss of feeling in the leg or foot. This often accompanies nerve irritation and can create challenges with maintaining sensory feedback, particularly in the lower limbs.
- Weakness: Difficulty lifting the foot or maintaining balance due to nerve-related muscle weakness. This weakness can extend to the ankle or calf, causing instability when walking or standing.
- Mobility Challenges: Pain that worsens with prolonged sitting, standing, or sudden movements. These limitations often result in a reduced ability to participate in physical activities or complete routine tasks comfortably, leading to frustration and decreased quality of life.
Osteopathy for Sciatica
Osteopathy takes a comprehensive approach to sciatica, focusing on the interconnectedness of the body’s systems. By addressing alignment, mobility, and nerve irritation, osteopathy can alleviate pain and improve overall function. Unlike other treatments that often target symptoms in isolation, osteopathy examines how the entire body works together to maintain balance and function, providing a holistic perspective on recovery.
Techniques Osteopaths Use
- Soft Tissue Therapy: This involves gently relieving tension in muscles that may be compressing or irritating the sciatic nerve. This technique also improves circulation, helping to reduce inflammation and support the body’s natural healing process.
- Spinal Mobilization: Adjusting the alignment of the spine reduces pressure on the nerve and promotes better disc health. This process not only alleviates pain but also restores flexibility and enhances the overall stability of the spine.
- Postural Adjustments: Osteopaths work to correct imbalances in posture and movement patterns that may contribute to sciatica. By addressing habits that place strain on the sciatic nerve, this technique prevents recurrence and promotes healthier biomechanics over time.
In addition to these techniques, osteopaths often incorporate education and advice to empower patients with knowledge about their condition. These personalized treatment plans are designed to address the root cause of pain, reduce the risk of future issues, and improve overall quality of life.

Practical Tips for Managing Sciatica
In addition to osteopathic treatment, incorporating simple lifestyle changes can help manage sciatica symptoms. Small adjustments in your daily routine can have a profound impact on alleviating discomfort and preventing future flare-ups. By staying proactive, you can regain control over your movement and quality of life.
- Stretch Regularly: Focus on stretches that target the lower back, hips, and hamstrings to relieve tension. Incorporate dynamic stretches to warm up before physical activities and static stretches to cool down after exercise. These practices enhance flexibility and reduce muscle stiffness.
- Ergonomic Adjustments: Use supportive chairs, maintain proper posture, and ensure your sleeping position minimizes strain on your back. Consider adding lumbar support cushions for chairs or investing in an adjustable desk to reduce pressure on the lower spine during long periods of sitting.
- Gentle Movement: Engage in low-impact activities like walking or swimming to keep the body active and improve circulation. These exercises not only ease stiffness but also stimulate endorphin release, helping to naturally reduce pain. Incorporating yoga or Pilates can further enhance core strength and stability, providing additional support to the lower back.
FAQs About Sciatica and Osteopathy
What causes sciatica to flare up?
Activities that put pressure on the lower back or nerve, such as prolonged sitting, heavy lifting, or poor posture, can trigger flare-ups. Emotional stress and fatigue can also exacerbate symptoms by increasing muscle tension, further irritating the nerve. Identifying and managing these triggers is an essential part of long-term relief.
How long does it take to recover from sciatica?
Recovery times vary depending on the severity of the condition and the treatment approach. Many patients see improvement within a few weeks of osteopathic care. However, chronic cases may require ongoing management, combining hands-on treatment with lifestyle adjustments to ensure sustained progress. Patience and consistency are key to achieving optimal results.
Can osteopathy prevent sciatica from recurring?
Yes, by addressing underlying causes such as posture, muscle imbalances, and spinal alignment, osteopathy can reduce the likelihood of recurrence. Regular maintenance treatments and adopting ergonomic habits can further strengthen the body’s resilience. Education provided by osteopaths helps patients make informed decisions to minimize future risks and maintain long-term spinal health.
Is sciatica a lifelong condition?
Not necessarily. While sciatica can become chronic if left untreated, many individuals find long-term relief with the right combination of care and lifestyle adjustments. Osteopathy addresses root causes, helping to alleviate symptoms and prevent recurrence, enabling many patients to return to their normal routines.
What lifestyle changes help manage sciatica?
Maintaining an active lifestyle with regular exercise, using proper ergonomics at work and home, and incorporating stress-management techniques like mindfulness or yoga can significantly reduce symptoms. Osteopaths often provide tailored advice to help integrate these changes effectively.
Sciatica can be a debilitating condition, but it doesn’t have to define your life. Left untreated, sciatica can lead to chronic pain, reduced mobility, and a cycle of discomfort that affects not just your physical health but also your mental and emotional well-being. However, with the right approach, relief is within reach.
At The Barefoot Osteo Warrnambool, we specialize in providing holistic and sustainable solutions to pain relief, focusing on the root causes rather than temporary fixes. By addressing alignment, mobility, and nerve function, our osteopathy services empower patients to take control of their health and regain their ability to move freely. Beyond pain relief, osteopathic care fosters resilience and supports the body’s natural healing mechanisms, offering a pathway to lasting wellness.
Take the first step toward relief. Book your consultation in Warrnambool today and discover how osteopathy can help you find lasting relief from sciatica pain. Embrace a future of improved mobility, reduced discomfort, and renewed confidence in your ability to live life fully.
References:
Baloh, R. W. (2019). Initial management of sciatica. In Sciatica and chronic pain (pp. 1–10). Springer, Cham.
Bernstein, I. A., Malik, Q., Carville, S., & Ward, S. (2017). Low back pain and sciatica: Summary of NICE guidance. BMJ, 356, i6748.
Boyajian-O’Neill, L., McClain, R., Coleman, M. & Thomas, P. (2008). Diagnosis and Management of Piriformis Syndrome: An Osteopathic Approach. Journal of Osteopathic Medicine, 108(11), 657-664.
Inman, J., & Thomson, O. P. (2019). Complementing or conflicting? A qualitative study of osteopaths’ perceptions of NICE low back pain and sciatica guidelines in the UK. International Journal of Osteopathic Medicine, 31, 7–14.
Koes, B. W., van Tulder, M. W., & Peul, W. C. (2007). Diagnosis and treatment of sciatica. BMJ, 334, 1313.
Konstantinou, K., & Dunn, K. M. (2008). Sciatica: Review of epidemiological studies and prevalence estimates. Spine, 33(22), 2464–2472.
Lewis, D. & Summers, G. (2017). Osteopathic Manipulative Treatment for the Management of Adjacent Segment Pathology. Journal of Osteopathic Medicine, 117(12), 782-785.
Ropper, A. H., & Zafonte, R. D. (2015). Sciatica. New England Journal of Medicine, 372(13), 1240–1248.
Valat, J.-P., Genevay, S., Marty, M., Rozenberg, S., & Koes, B. (2010). Sciatica. Best Practice & Research Clinical Rheumatology, 24(2), 241–252.
Vroomen, P. C. A. J., de Krom, M. C. T. F. M., Slofstra, P. D., & Knottnerus, J. A. (2000). Conservative treatment of sciatica: A systematic review. Journal of Spinal Disorders, 13(6), 463–469.









